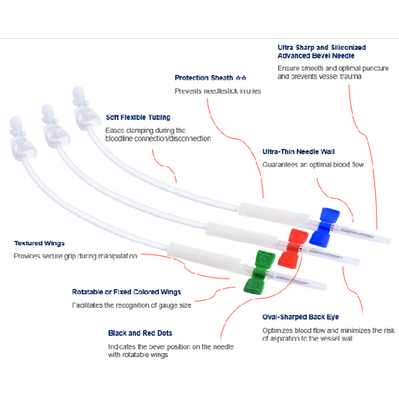
Supercath™ Plastic Cannula Needles
The gold standard of needles for enhanced patient comfort and preserving fistula health
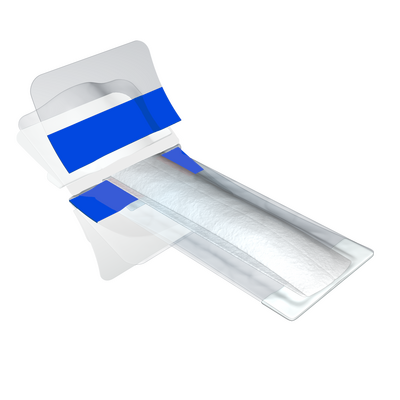
Supercath™ PRO plastic dialysis cannula comes with a fully encased passive safety mechanism with a built-in non-return (check) valve that prevents the backflow of blood and allows the blood line connection without clamping.
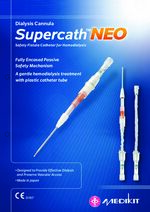
Supercath™ NEO features the same fully encased passive safety mechanism, protecting users from sharps injury, but without the non-return (check) valve.
For a gentle treatment
A gentle treatment with a plastic catheter cannula that centralises itself in the vein using multiple ports.
Supercath™ NEO features the same fully encased passive safety mechanism, protecting users from sharps injury, but without the non-return (check) valve.
For a gentle treatment
- Protection from injuries to the vessel wall
- For patients on nocturnal, home or long dialysis
- For a more comfortable treatment
- Protection of needlestick injuries
- Protection of and blood exposure/infectious blood
- with tortuous and deeply located vessels
- with special movement needs (anxious or restless patients - e.g. dementia or mental health problems)
- with metal allergies
- For patients with a new fistula (early cannulation)
- To protect and preserve the AVF/ AVG
A gentle treatment with a plastic catheter cannula that centralises itself in the vein using multiple ports.
| Product Code | Plastic Fistula Cannula Needles (soft needles for arterial & venous site use) | Gauge | Needle Length mm |
|---|---|---|---|
| SP802-14 (25) | Supercath NEO soft safety fistula cannula 14G - 25mm cannula, protector sheath | 14 | 25 |
| SP802-15 (25) | Supercath NEO soft safety fistula cannula 15G - 25mm cannula, protector sheath | 15 | 25 |
| SP802-16 (25) | Supercath NEO soft safety fistula cannula 16G - 25mm cannula, protector sheath | 16 | 25 |
| SP402-14 (25) | Supercath PRO soft safety fistula cannula 14G -25mm cannula, protector sheath, non-return valve | 14 | 25 |
| SP402-14 (33) | Supercath PRO soft safety fistula cannula 14G - 33mm cannula, protector sheath, non-return valve | 14 | 33 |
| SP402-15 (25) | Supercath PRO soft safety fistula cannula 15G - 25mm cannula, protector sheath, non-return valve | 15 | 25 |
| SP402-15 (33) | Supercath PRO soft safety fistula cannula 15G - 33mm cannula, protector sheath, non-return valve | 15 | 33 |
| SP402-16 (25) | Supercath PRO soft safety fistula cannula 16G - 25mm cannula, protector sheath, non-return valve | 16 | 25 |
| SP402-16 (33) | Supercath PRO soft safety fistula cannula 16G - 33mm cannula, protector sheath, non-return valve | 16 | 33 |
| SP402-17 (25) | Supercath PRO soft safety fistula cannula 17G - 25mm cannula, protector sheath, non-return valve | 17 | 25 |
| SP402-17 (33) | Supercath PRO soft safety fistula cannula 17G - 33mm cannula, protector sheath, non-return valve | 17 | 33 |
Clinical Information:
The Use of Plastic Cannula Needles for Vascular Access in Haemodialysis
Summary of Published Data
Introduction
Plastic cannula needles in haemodialysis have gained attention due to their potential to reduce complications and improve patient outcomes compared to traditional metal needles. This document discusses the findings from various clinical studies and reviews the benefits, challenges, and economic implications associated with the adoption of plastic cannula needles in haemodialysis.
Clinical Evidence and Findings
- Dynamic Arterial and Venous Pressure Studies
- Choi et al. (2020) conducted a study comparing the dynamic arterial and venous pressures between metal needles and plastic cannulas in incident haemodialysis patients with arteriovenous grafts (AVGs). The study found that plastic cannulas resulted in less negative arterial pre-pump pressures and lower venous pressures at all prescribed blood flow rates compared to metal needles. This indicates more stable pressure dynamics with plastic cannulas, which can reduce vascular trauma and improve access outcomes.
- Early Cannulation and AVF Patency
- Shi et al. (2019) analysed the effect of early cannulation with plastic cannulas on the patency of arteriovenous fistulas (AVFs). The study concluded that early cannulation (less than 10 days post-creation) did not negatively affect AVF patency. This finding suggests that plastic cannulas can be used for early cannulation without compromising vascular access, potentially reducing the need for temporary central venous catheters.
- Economic Benefits and Cost-Effectiveness
- Tito et al. (2022) evaluated the costs associated with managing complications in haemodialysis patients and the potential savings from using plastic cannula needles. The study highlighted significant cost savings by reducing the incidence of complications such as infections, hematomas, and thrombosis. The analysis indicated that the reduction in treatment costs for complications offsets the higher upfront cost of plastic cannulas.
- Experience in Spanish Haemodialysis Units
- A review in the Journal of Renal Care (2020) discussed the experiences of Spanish haemodialysis units using plastic cannulas. The findings reported fewer complications and improved patient comfort, further supporting the clinical benefits of plastic cannulas over metal needles.
- Cannulation Practices and Challenges
- Kumbar et al. (2018) reviewed cannulation practices and highlighted the benefits of plastic cannulas, especially in patients with delicate fistulas, tortuous vessels, or metal allergies. The study also pointed out the need for proper training and technique adaptation to maximise the benefits of plastic cannulas.
- Feasibility and Resistance to Adoption
- A 2022 feasibility crossover randomised trial (Fielding et al.) involving eight patients found that plastic cannula were feasible in prevalent haemodialysis patients; however, centres that historically used metal needles showed resistance to change. Additionally, a 2023 international survey indicated a preference for metal needles among dialysis nurses despite evidence of lower adverse events in certain patient populations using plastic cannula.
- Additional Economic and Clinical Insight
- A recent study presented at ISPOR Europe 2024 (Ghosh et al.) further examined plastic cannula needles' cost-effectiveness and clinical benefits. The findings emphasised the economic advantages of plastic cannulas, including reduced hospitalisation rates due to fewer complications. It concluded that
Discussion
Advantages of Plastic Cannula Needles
- Reduced Complications: Plastic cannulas are associated with lower rates of complications such as hematomas, infiltrations, infections, and thrombosis. Their flexible nature reduces trauma to the vessel wall, minimising the risk of these adverse events.
- Improved Vascular Access Outcomes: The stable arterial and venous pressures maintained by plastic cannulas enhance the longevity and functionality of vascular access sites. This is particularly beneficial for AVFs and AVGs, which are critical for effective haemodialysis.
- Economic Efficiency: While plastic cannulas may have a higher initial cost, the overall savings from reduced complication rates and fewer interventions make them a cost-effective choice for haemodialysis units. The economic benefits extend to both healthcare providers and patients, reducing the financial burden associated with vascular access complications.
Challenges and Barriers
- Training and Adaptation: Successful implementation of plastic cannulas requires proper training for healthcare staff. The cannulation technique differs from that of metal needles, necessitating adjustments in practice to ensure optimal outcomes.
- Patient and Staff Acceptance: Patients and healthcare providers can resist the adoption of new devices. Addressing concerns and providing education on the benefits and proper use of plastic cannulas is crucial to ensuring acceptance and compliance.
- Availability and Supply: Ensuring a consistent supply of plastic cannulas and managing inventory can be a logistical challenge. Healthcare facilities need to establish reliable procurement processes to avoid disruptions in the availability of these devices.
Conclusion
Adopting plastic cannula needles in haemodialysis offers significant clinical and economic benefits. Clinical studies have demonstrated their potential to reduce complications, improve vascular access outcomes, and provide cost savings. However, successful implementation requires addressing challenges related to training, acceptance, and supply management. Overall, plastic cannulas represent a valuable advancement in the management of vascular access in haemodialysis, promising better patient outcomes and more efficient use of healthcare resources.
- Choi et al. (2020). Comparison of dynamic arterial and venous pressure between metal needles and plastic cannulas in incident haemodialysis patients with arteriovenous grafts. The Journal of Vascular Access.
- Shi et al. (2019). Effect of early cannulation with plastic cannula on arteriovenous fistula patency in haemodialysis patients. Blood Purif.
- Tito et al. (2022). Haemodialysis patients and complications management costs in Italy: plastic cannulae as a potentially cost-effective alternative. Journal of Vascular Access.
- Analysis of experience of the use of plastic cannulas in Spanish haemodialysis units. (2020). Journal of Renal Care.
- Kumbar et al. (2018). Fistula Cannulation with a Novel Fistula Cannula: A Review of Cannulation Devices and Procedures. Blood Purif.
- Fielding, C. A., Hadfield, A., White, K., Waters, D., James, C., Buchanan, H., Fluck, R. J., & Selby, N. M. (2022). The use of haemodialysis plastic cannula in prevalent patients with kidney failure: A feasibility crossover randomised trial study. Journal of Vascular Access, 23(2), 112–118.
- Ghosh, P., Ahmed, S., Hepworth, C., Greenhough, B., Barth, C., & Blömeke, L. (2024). Metal needles versus plastic cannulae in haemodialysis patients: A cost-benefit analysis. ISPOR Europe 2024 Conference.
Images - Click to enlarge